A SOAP note is a structured medical document that records a patient's condition and history through four parts:
- Subjective
- Objective
- Assessment
- Plan
Its purpose is to organize care details in a clear and reliable way so every team member can understand what has been done and what still needs attention. Writing an example of a SOAP note helps students understand how healthcare documentation works.
If you're trying to juggle your other assignments along with your medical school homework, you can rely on writers from EssayService for real guidance.

What Is a SOAP Note?
A SOAP note is a written medical document with four clear parts. The Subjective section records patient statements and personal descriptions of symptoms. The Objective section lists measurable findings, such as vital signs or lab data. The Assessment section includes the clinician's interpretation of these findings. The Plan section outlines future actions for treatment or follow-up. Each part serves a purpose. Together, they create a complete view of the patient's current condition and care plan.
If you’re working on your school assignments, check out our list of nursing research topics to find inspiration for your paper.
How Long Is a SOAP Note?
A nursing SOAP note usually stays brief. Most sections fit within one or two short paragraphs. The length depends on the situation. A routine visit often requires only a few sentences, while a complex case may need more space for detail. Each section must include enough information to guide the next provider without slowing them down.
A strong nursing SOAP note remains focused, mostly on the important details about the patient's condition and helps every nurse or doctor stay on the same page during each shift.
How to Write a SOAP Note: Writing Steps with Examples
Learning how to use a SOAP note format begins with understanding its structure. Each part mentions a specific kind of information that tells you about the client's health and progress. The steps below show how to build a note that feels practical and useful for every clinician who reviews it.
Step 1: Record the Subjective Section
This section gathers what the client reports during the session. It focuses on their words, thoughts, and feelings. Write about the main concern or the presenting problem. Include the client's chief complaint if one is stated clearly.
Example: The client presented with difficulty concentrating. They expressed frustration about recurring headaches over the past week and described disrupted sleep patterns.
Step 2: Write the Objective Section
This part documents what can be seen or measured. Include observable behavior, clinical findings, and any data collected during the visit. Record vital signs in clear terms. Mention how the client interacts during a discussion or a therapy session, if it helps show their current state.
Example: Blood pressure measured 130 over 85 mmHg. The client made steady eye contact throughout the conversation. They appeared alert and actively participating in the process.
Step 3: Add the Assessment Section
The assessment combines the subjective and objective information gathered in the previous parts. All of them help you form a professional interpretation of data. This is the time for clinical reasoning. Note what the findings suggest and describe how symptoms connect to a broader diagnosis.
Example: Current symptoms and behaviors point to generalized anxiety disorder. The client experiences distress linked to ongoing academic pressures and limited coping strategies.
Step 4: Develop the Plan Section
This step defines the treatment plan in clear, actionable terms. Outline what will happen next. Mention steps for the next session and goals for the upcoming session. Include specific activities or techniques that guide progress. Add details about additional testing or specialist referral if needed.
Example: Introduce relaxation techniques such as deep breathing and progressive muscle relaxation. Assign homework to practice mindfulness techniques daily before the next session.
SOAP Note Template in PDF Format
A complete SOAP note follows a simple layout where each section stands on its own. The SOAP note outline divides the document into four main parts:
- Subjective: Records client reports, personal descriptions, and relevant symptoms shared during the session.
- Objective: Lists measurable data, observed behaviors, and clinical findings gathered through examination.
- Assessment: Summarizes professional interpretations and outlines how the findings connect to the condition.
- Plan: Details future steps, follow-up care, and any actions that guide the next stage of treatment.
Take a look at the sample in PDF format below to see how the four parts we just described look on paper:
SOAP Notes Examples
SOAP notes adapt to the needs of each profession, yet the framework stays unchanged. Looking through specific examples will help you strengthen SOAP note practice, since each one shows how the specific details change from one field to another.
SOAP Note Example for Speech Therapy
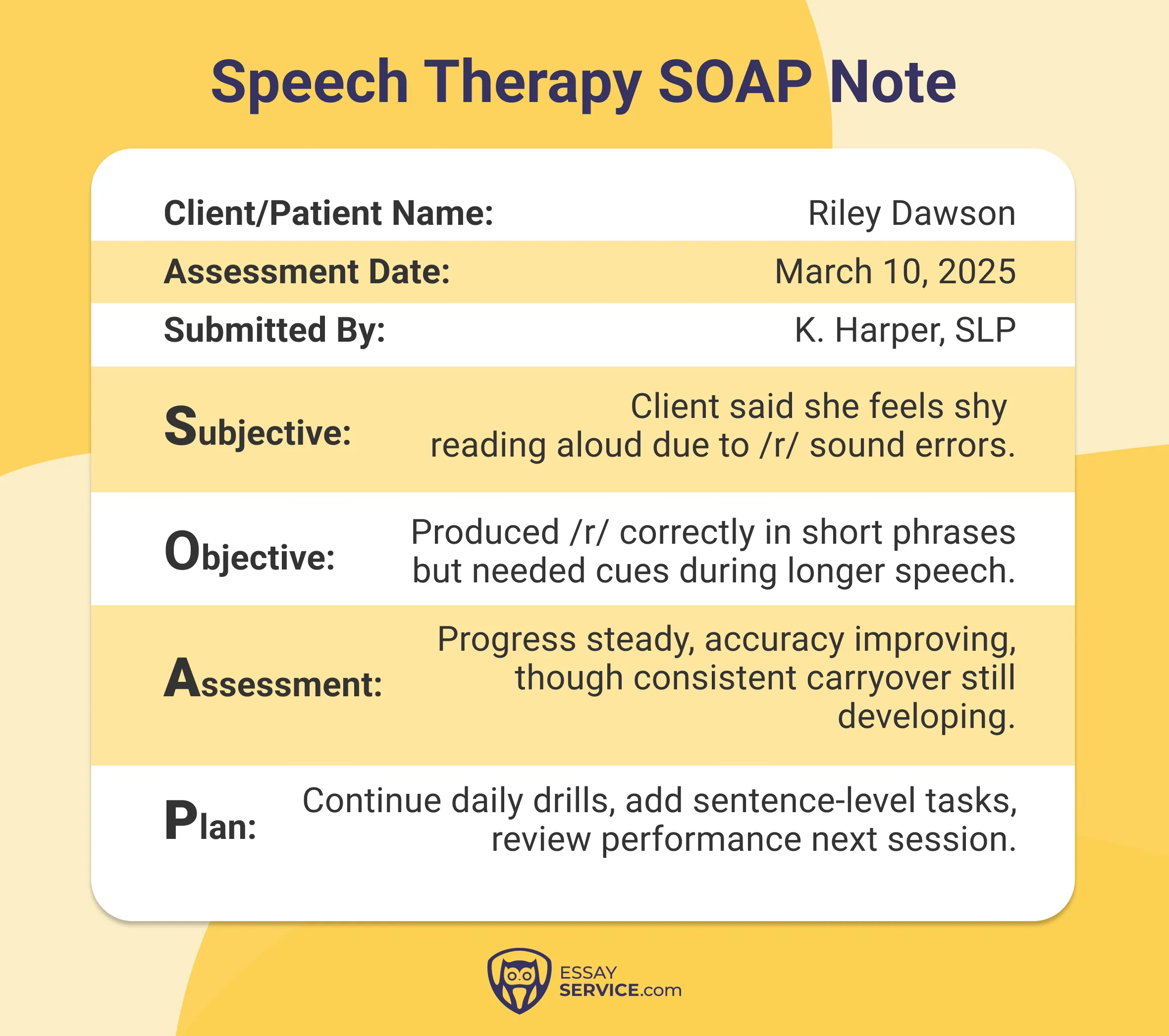
This example works because the note stays anchored in one clear articulation goal. Each part serves a purpose. The Subjective section sets the scene with a short account of the client's experience. The Objective captures a single measurable skill. The Assessment links progress to technique, while the Plan extends learning into simple, repeatable exercises.
Mental Health SOAP Note Example
%20Mental%20Health%20SOAP%20Note.webp)
This is one of the clearest sample SOAP notes, which succeeds by balancing emotion with structure. The Subjective gives voice to what the client feels. The Objective keeps focus on what can be seen or confirmed. The Assessment pulls both together, outlining steady growth. The Plan then turns those insights into specific actions that build confidence over time.
SOAP Note Example for Occupational Therapy
%20Occupational%20Therapy%20SOAP%20Note.webp)
This version stands out for its attention to daily function. The Subjective reflects personal motivation and small victories. The Objective shows exactly what tasks were performed and how well they went. The Assessment interprets progress through skill development. The Plan lists activities that strengthen independence beyond the clinic.
SOAP Note Example for Massage Therapy
%20Massage%20Therapy%20SOAP%20Note.webp)
This model shines through clarity and observation. The Subjective notes where tension exists and how it feels. The Objective details what was found during palpation and how the tissue responded. The Assessment identifies patterns behind discomfort. The Plan closes with precise suggestions that match what was seen on the table.
SOAP Note Example for Physical Therapy

This example demonstrates disciplined recordkeeping. The Subjective highlights perceived strain or fatigue. The Objective documents measurable change in strength or mobility. The Assessment weighs these results against treatment goals. The Plan maps out the next stage of movement, one step at a time.
Counseling SOAP Note Example

This note works because it traces the growth of insight, not just emotion. The Subjective captures what the client realized or struggled to articulate. The Objective records tone, focus, and participation. The Assessment outlines shifts in thinking. The Plan uses that understanding to shape new reflective exercises.
SOAP Note Example for Individual Psychotherapy
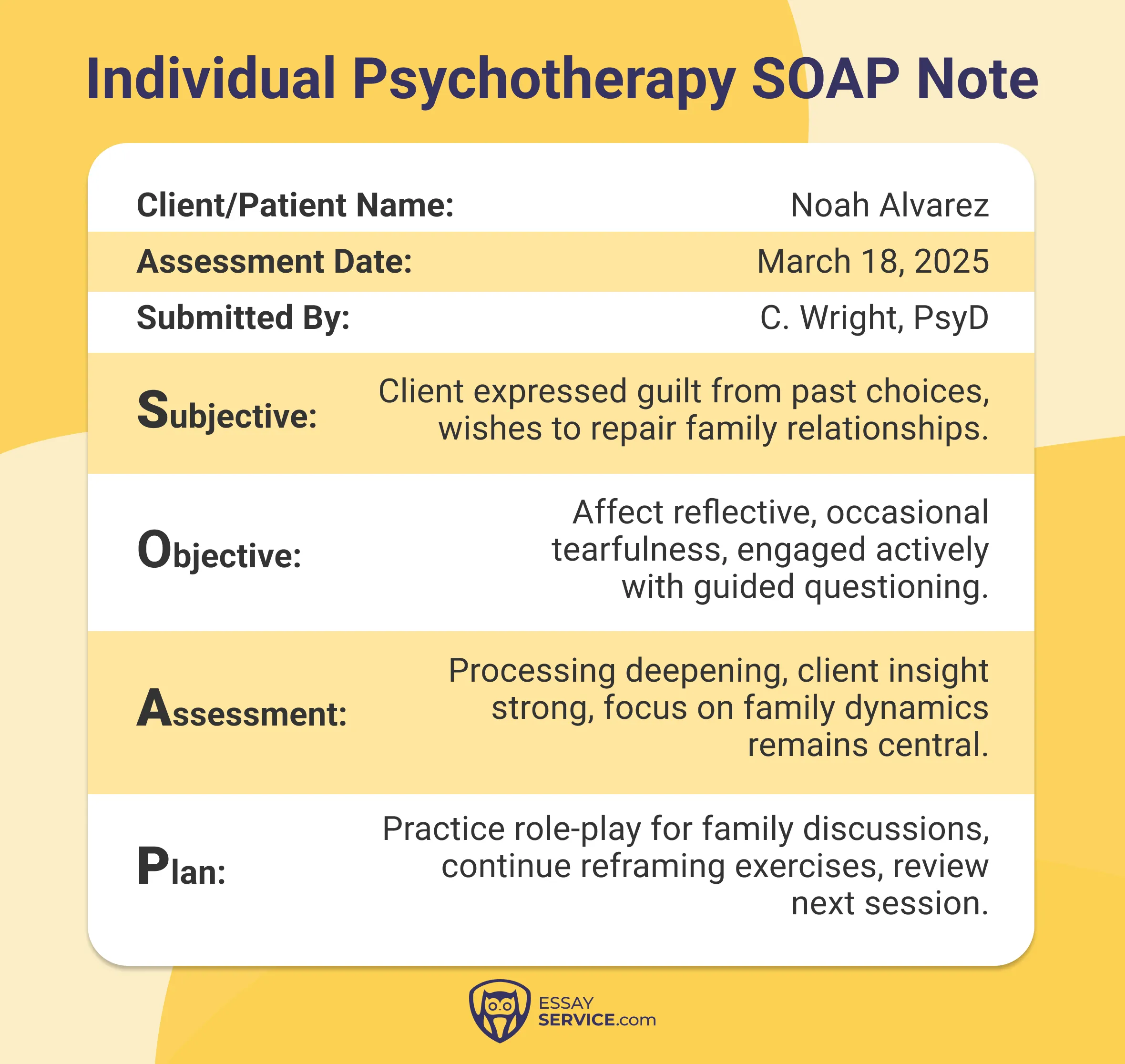
This version reads with depth and precision. The Subjective recounts personal reflection and emotional honesty. The Objective provides neutral evidence of engagement and composure. The Assessment connects inner awareness to outward behavior. The Plan offers tools that continue emotional work beyond the session.
Psychiatry SOAP Note Example
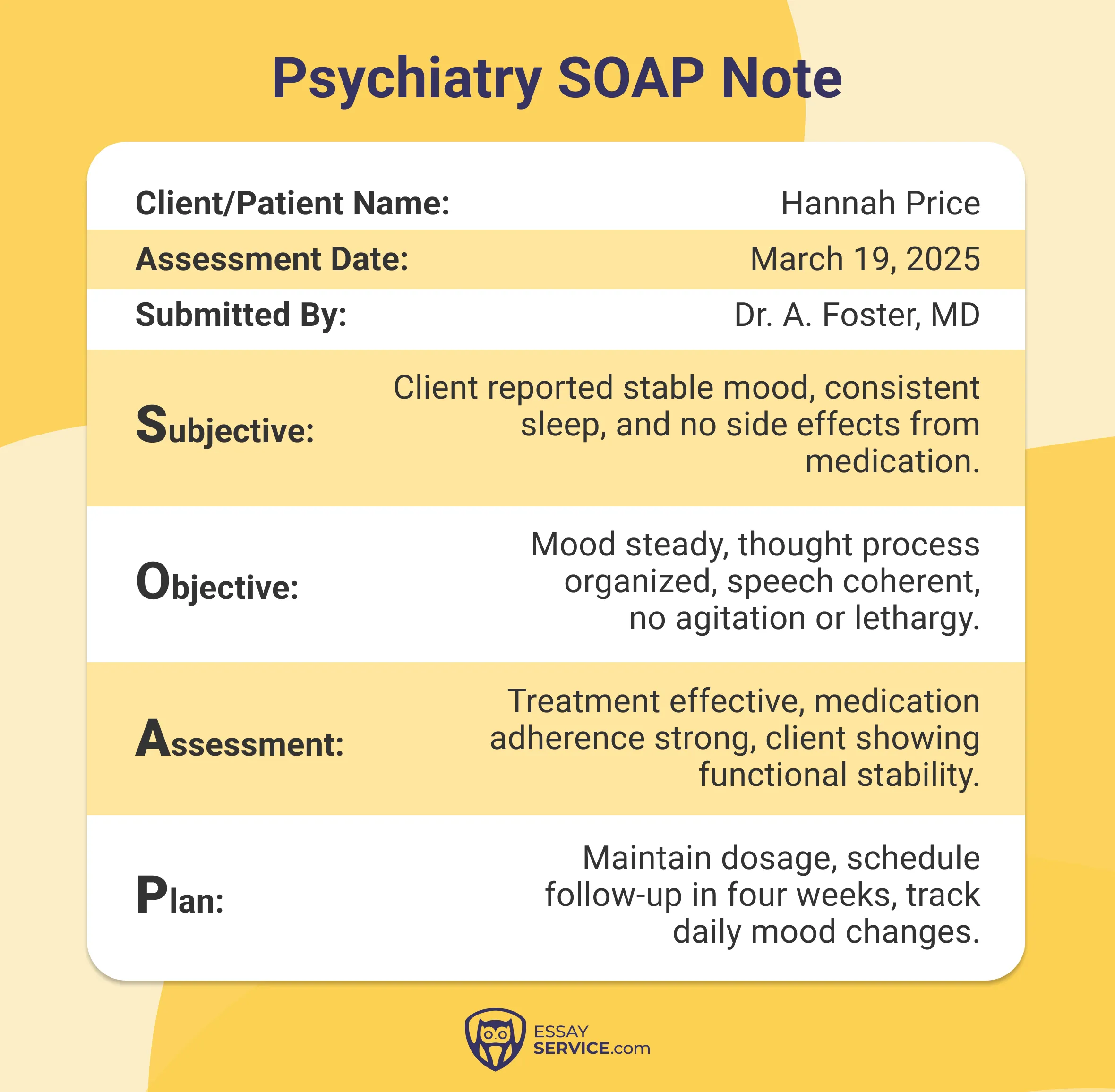
This model holds together through factual precision. The Subjective states how the client feels under the current medication. The Objective records mental clarity, energy, and concentration. The Assessment evaluates the medication's effect on stability. The Plan details adjustments or confirms that no change is needed.
Bipolar Disorder SOAP Note Example
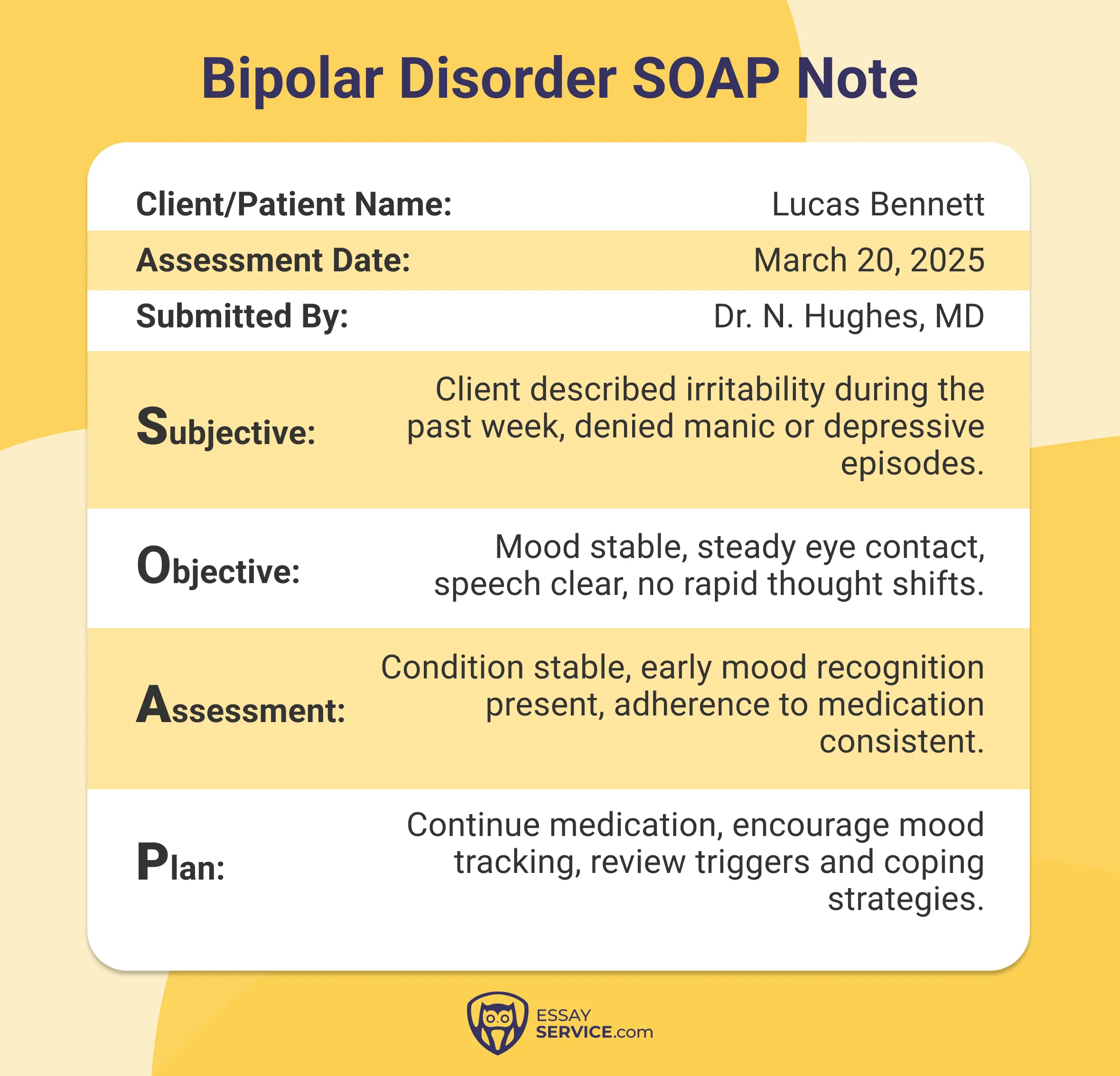
This note is effective because it follows patterns over time. The Subjective covers mood changes and routine consistency. The Objective verifies steadiness through observed behavior. The Assessment interprets these signs within the larger treatment timeline. The Plan reinforces habits that sustain balance.
Eating Disorder SOAP Note Example

This example stands out for linking structure to progress. The Subjective includes reflections on eating experiences. The Objective reports adherence to scheduled meals and participation in support work. The Assessment identifies emerging stability. The Plan builds on this foundation with realistic goals for continued recovery.
Expert Tips for Writing SOAP Notes
Writing SOAP notes requires accuracy, patience, and consistency. Each entry reflects your professionalism and helps other healthcare providers understand your work. Keep these habits in mind as you write:
- Start by focusing each section on relevant information. Avoid adding subjective opinions that don't contribute to care decisions.
- Follow a consistent format for every entry so other providers can easily locate details and follow updates.
- Write measurable information wherever possible. Describe what can be seen, heard, or tested to support each observation.
- Review every note before closing it. Make sure the content is clear and supports continuity of care.
- Use simple, direct language to ensure effective communication across teams.
Benefits of Using the SOAP Notes Format
The SOAP notes format has many different benefits across areas of healthcare. For example:
- Structured Organization: Keeps information orderly so every client encounter follows the same layout.
- Consistent Progress Tracking: Makes it easier to compare visits, trace client progress, and record changes in condition.
- Goal Alignment: Helps clinicians set treatment goals that remain visible and measurable across sessions.
- Improved Workflow: Allows healthcare providers to scan earlier notes, review objective data, and understand how each condition evolved.
- Collaborative Care: Builds genuine teamwork. It keeps every provider aligned through shared notes that speak the same language. This approach also allows families to understand what's happening.
- Accurate Assessment: Supports clinical reasoning. Each entry becomes a record of clear reasoning, steady observation, and purposeful action.
- Legal Reliability: A well-written note stands as proof of professional integrity. It meets documentation standards with precision and transparency.
Bringing It All Together
Each entry of SOAP notes shows a specific moment in care: what was observed and what decisions took shape. The structure helps clinicians bring more order to complicated cases. Also, it's needed for the next provider to understand the patient's condition without confusion.
For students still learning how to build a precise SOAP note, EssayService can make the process easier with guidance tailored to healthcare learners. If you’re just now trying to get into medical school, a quick look at nursing personal statement examples can help you strengthen your application.
Frequently Asked Questions
Is There a Standard SOAP Note Template?
Yes. Most healthcare settings use a familiar structure that guides both writing and review. The note unfolds across four distinct parts, where each one focuses on a single function.
What Are the 4 Parts of the SOAP Method?
The SOAP method divides documentation into four sections. Each one handles a different layer of information.
- Subjective: Write what the client describes in their own words. This might include discomfort, emotional distress, or changes they have noticed in daily routines.
- Objective: Record what can be measured. Add test results, physical findings, or behaviors seen during the session. Keep this section factual and concise.
- Assessment: Combine the information into a professional conclusion. Explain what the data suggests and how it shapes the understanding of the client's condition.
- Plan: Describe what will follow. Outline new interventions, treatment adjustments, or scheduled follow-up visits.
How Do You Write SOAP Notes?
Begin with careful listening. Collect the client's account before adding your observations. Sort each detail into the correct section so the note reads in a logical order. Use clear sentences. Remove any filler or repetition. Each entry should help the next provider understand the situation and what steps to take.
What Is an Example of a SOAP Note?
Imagine a client talking about sharp knee pain after finishing a workout. Build the note in four layers.
- Subjective: Record their description of the pain and note when it started. Mention how it changed their ability to walk or climb stairs.
- Objective: Write what you observed. Point out swelling around the joint. Add measurements that show limits in the range of motion.
- Assessment: Interpret these signs. The findings may suggest a mild strain. They may also reflect stress from overuse.
- Plan: Set a direction for care. Recommend rest for a short period. Add gentle stretching exercises. Arrange a follow-up appointment to monitor healing.
What Are Some Common SOAP Note Mistakes?
Writers often blend facts with personal interpretation. This weakens clarity. Others leave out small updates that reveal changes between visits. A reliable note keeps each part separate. It states what was heard, seen, and what those details mean. Finally, it marks what actions will improve patient care.

Susan shapes the new generation of nursing professionals as a professor. Her medical degree and teaching experience make for a wealth of advice on researching and writing complex papers.
- What Are SOAP Notes in Nursing + Examples. (2025). https://nurse.org/education/soap-notes-nursing/
- APSU Writing Center. (2024). SOAP note taking method. Austin Peay State University. https://www.apsu.edu/writingcenter/writing-resources/SOAP-Note-Taking-Method-2024.pdf
- Shumaker, W., jmm49, & djd139. (n.d.). Chapter 07: SIMPLE SOAP – NOTE EXAMPLES. https://psu.pb.unizin.org/psushptamedicaldocumentation/chapter/chapter-7/
New posts to your inbox
Your submission has been received!


.png)
.png)